Today, cervical cancer remains a significant cause of cancer morbidity and mortality among women. In fact, in 2020, cervical cancer was the fourth most common cancer in women worldwide. Fortunately, due to access to cervical cancer screening and prevention programs, the U.S experienced a significant decrease in cervical cancer deaths compared to the rest of the world. In the past 50 years, there has been a 75% decrease in cervical cancer incidence and mortality in countries that have implemented screening and prevention programs. For this reason, Canyon View highly encourages regular screening and vaccination against cervical cancer.
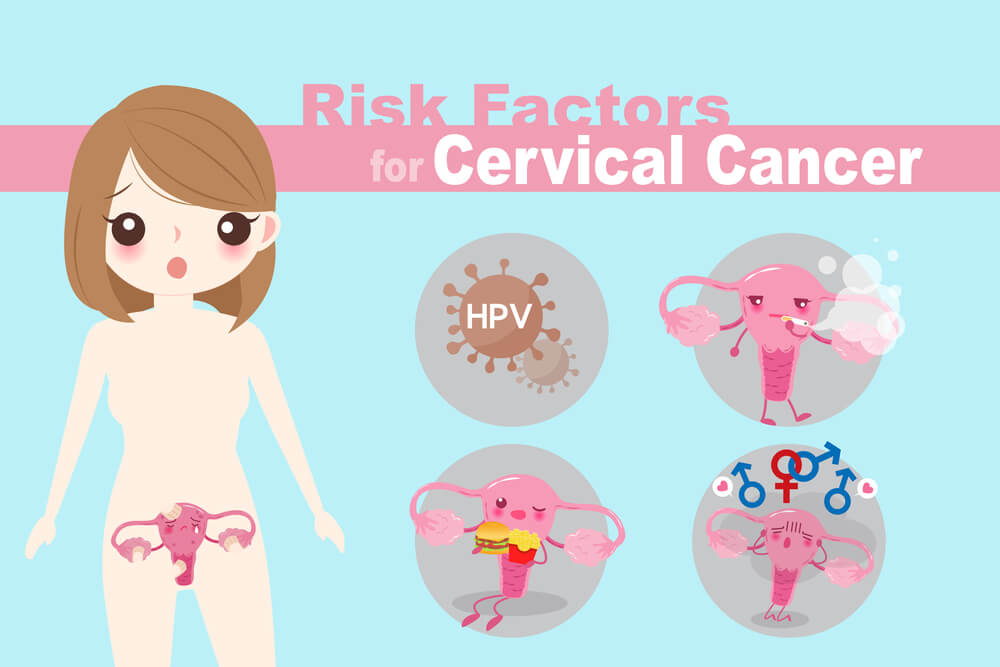
You may be wondering, what exactly is cervical cancer? Cervical cancer is cancer of the uterine cervix and thus, occurs only in women. Cervical cancer is almost always caused by human papillomavirus (HPV) infection. On rare occasions, it can be due to other non-HPV causes such as genetics, cigarette smoking, and even oral contraceptive use. Because cervical cancer is so frequently caused by HPV infection, it is essential to understand HPV. HPV is the most common sexually transmitted infection in the United States and is spread by vaginal, anal, or oral intercourse with someone who has HPV. It can cause cervical cancer and cancer of the vulva, vagina, penis, anus, and oropharynx. Different strains of HPV can cause genital warts as well. Because cancer from HPV takes years to develop after getting infected, it is difficult to know when someone got infected if they have had multiple sexual partners over the years.

You may now be wondering, how can I avoid contracting HPV and developing cervical cancer? You can do several things to protect yourself from developing cervical cancer. The first thing you can do is get the HPV vaccine. The CDC and American College of Obstetrics and Gynecology recommend HPV vaccination at age 11-12 and for everyone through the age of 26 if they have not yet been vaccinated. The HPV vaccine is recommended not only for females but also males since they can be carriers of the virus. HPV vaccination has been shown to work exceptionally well, as it is estimated to prevent more than 90% of HPV-attributable cancers.
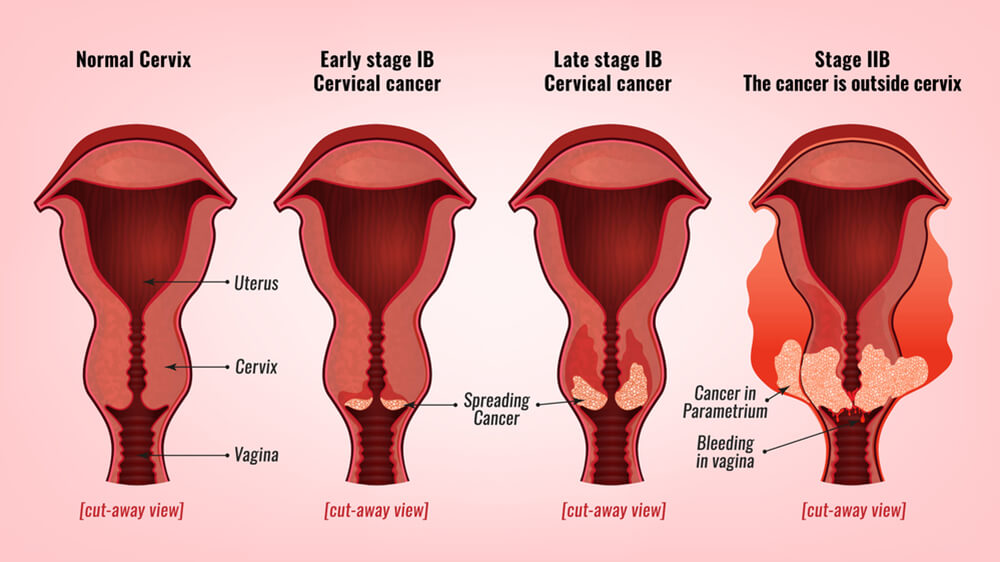
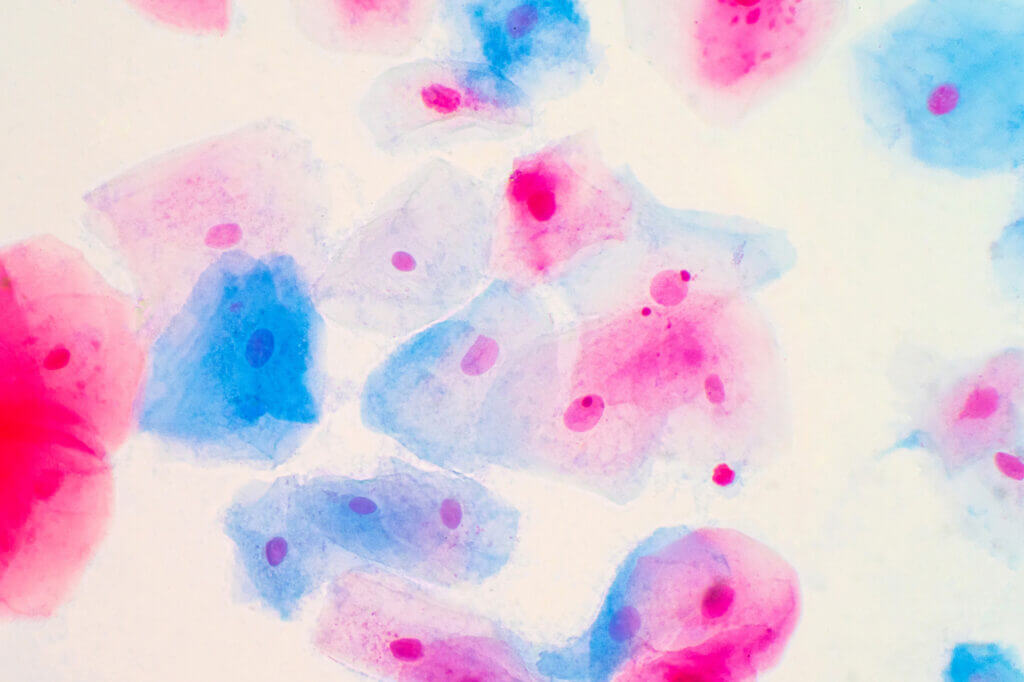
The second thing you can do to protect yourself is to get screened for cervical cancer. Screening for cervical cancer is recommended for all women ages 21 to 65 years old. Early screening for cervical cancer helps prevent the disease altogether. This can be done by getting a Pap test and/or HPV test. A Pap test checks for precancerous cells or changes of the cells in the cervix that might develop into cervical cancer, while the HPV test checks for the human papillomavirus that often causes those cells to change. Both of these tests can be done in your healthcare provider’s office. An instrument called a speculum is inserted through the vagina so your provider can examine your cervix and collect some cells and mucus from that area.
Screening with a Pap test is recommended every three years from age 21 to 29 years old. From ages 30 to 65, HPV testing is recommended every five years and a Pap test every three years. When both tests are done together, it is called “co-testing.” If your test results are typical for this test, your medical provider may recommend that you wait five years until your next screening. After the age of 65 or for women who have had a hysterectomy with removal of the cervix, screening is not recommended anymore if you have had normal previous results.
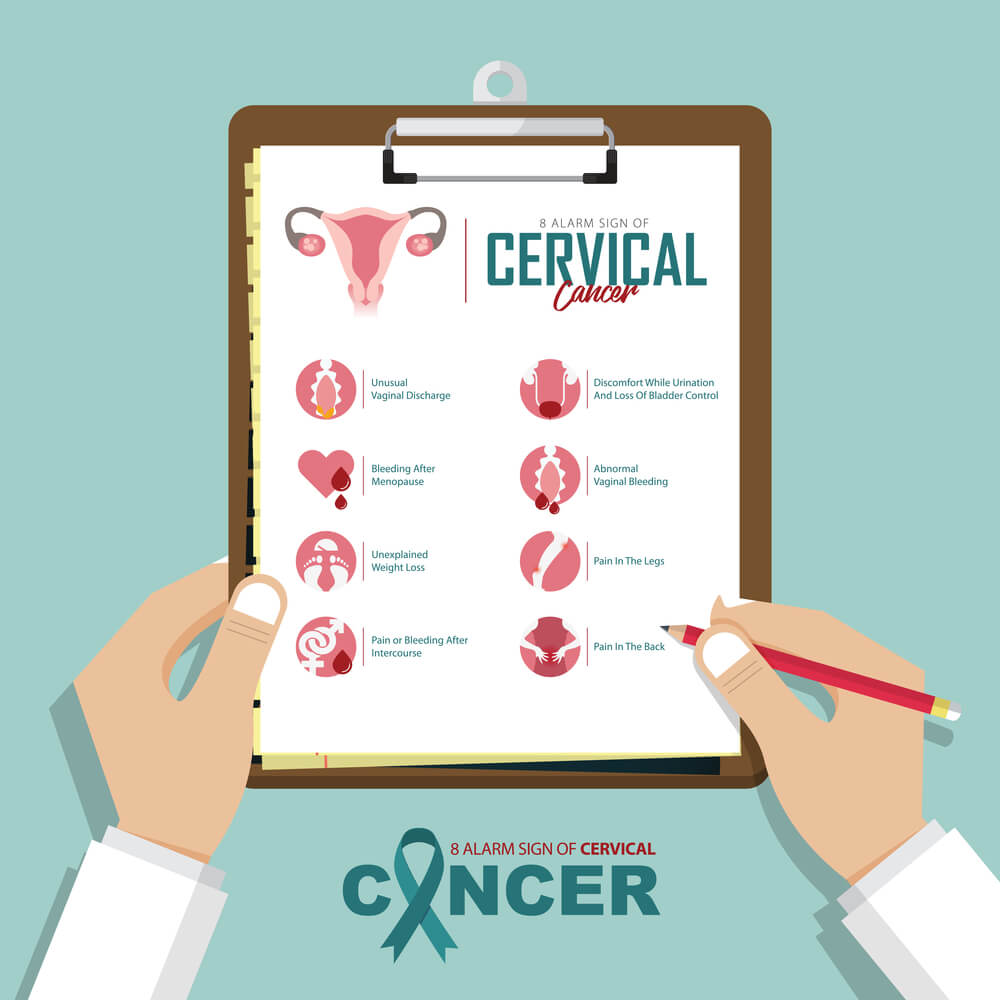
Screening for cervical cancer is an effective way to detect precancerous lesions and cancer. Because early cervical cancer is often asymptomatic, regular screening and HPV vaccination are critical aspects of one’s comprehensive reproductive health. Talk to your provider about your recommended screenings and vaccination schedule today.
Erin Tyrrell, FNP
Canyon View Family Medicine
Cervical Cancer: What should I know about screening? (2021). CDC. https://www.cdc.gov/cancer/cervical/basic_info/screening.htm
Invasive cervical cancer: Epidemiology, risk factors, clinical manifestations, and diagnosis. (2021). UpToDate. https://www.uptodate.com/contents/invasive-cervical-cancer-epidemiology-risk-factors-clinical-manifestations-and-diagnosis?search=cervical%20cancer%20&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H1
Updated Cervical Cancer Screening Guidelines. (2021). The American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2021/04/updated-cervical-cancer-screening-guidelines