Anemia is a word that you have probably heard many times, but maybe you aren’t exactly sure what it means. Perhaps you even know some of the symptoms, including feeling fatigued, or headaches. So, what is anemia? It starts with hemoglobin. Hemoglobin is a protein in your blood that carries oxygen. Iron is needed for your body to make hemoglobin. When hemoglobin is lower than normal, this is called anemia.
In nonpregnant females, hemoglobin less than 12 is considered anemic. Due to regular physiologic changes in pregnancy, a lower cut-off is used to diagnose anemia which varies by trimester. In the first and third trimesters, hemoglobin less than 11 is considered anemic, while 10.5 is used as the cut-off in the second trimester.
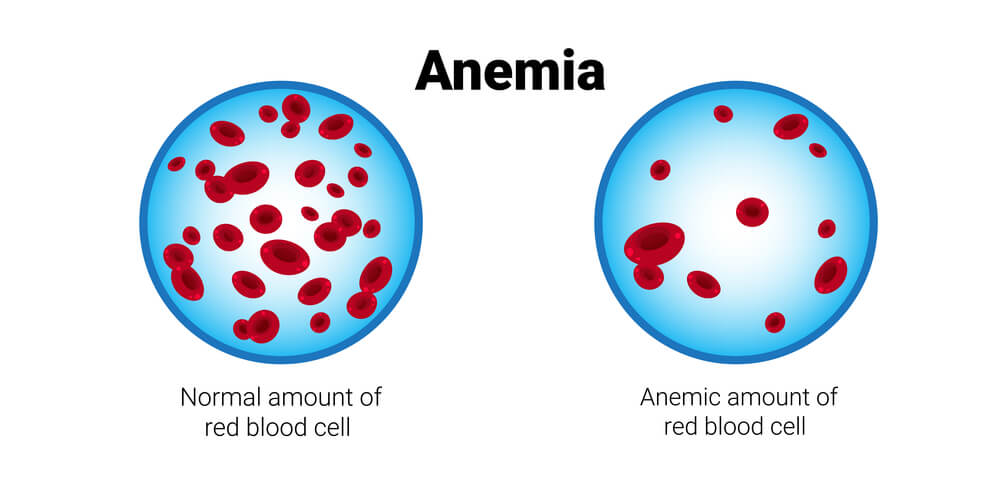
Anemia occurs in almost one-third of reproductive age women and up to 40% of pregnancies. The most common cause of anemia is not having enough iron available in your body to produce adequate hemoglobin levels. This is called iron-deficiency anemia.
The amount of iron your body needs in pregnancy varies a lot depending on your gestational age. At baseline, 1 mg per day is required for the normal turnover of red blood cells. In the first trimester, your needs increase to 2 mg per day and continue to increase up to 7 mg per day as you approach your due date. Iron can be found in many foods, including meat, lentils, beans, and spinach. Additionally, many foods are fortified with iron, such as fortified breakfast cereals and cream of wheat. Another good way to get more iron is through your prenatal vitamin.
For women diagnosed with iron-deficiency anemia, additional supplementation of iron either by mouth or intravenously (IV) may be recommended. Taking iron orally is easy and inexpensive but can cause a metallic taste, nausea, diarrhea, or constipation. Iron given through an IV is usually reserved for those who need more rapid iron replacement, such as those within a month of their due date, those who don’t tolerate oral iron supplementation, or those with a history of bariatric surgery, which can impair iron absorption.
Now that you know what anemia means and how common it is, you may feel a little worried about being anemic. You say to yourself, “I do feel tired! I do get headaches! Isn’t that part of being pregnant?” You are right! It might just be part of being pregnant. Rest assured, we routinely screen for anemia in pregnancy with your initial prenatal labs and again at the end of the second trimester when screening for gestational diabetes. This way, we can identify anemia appropriately and start treatment to resolve it.